


Currently, the world is facing a global health crisis unlike any other — COVID-19 is spreading human suffering, destabilizing the global economy and upending the lives of billions of people around the globe.
Before the pandemic, major progress was made in improving the health of millions of people. Significant strides were made in increasing life expectancy and reducing some of the common killers associated with child and maternal mortality. But more efforts are needed to fully eradicate a wide range of diseases and address many different persistent and emerging health issues. By focusing on providing more efficient funding of health systems, improved sanitation and hygiene, and increased access to physicians, significant progress can be made in helping to save the lives of millions.
Health emergencies such as COVID-19 pose a global risk and have shown the critical need for preparedness. The United Nations Development Programme highlighted huge disparities in countries’ abilities to cope with and recover from the COVID-19 crisis. The pandemic provides a watershed moment for health emergency preparedness and for investment in critical 21st century public services.
Facts and Figures:-
Child health
- In 2018 an estimated 6.2 million children and adolescents under the age of 15 years died, mostly from preventable causes. Of these deaths, 5.3 million occurred in the first 5 years, with almost half of these in the first month of life.
- Despite determined global progress, an increasing proportion of child deaths are in Sub-Saharan Africa and Southern Asia. Four out of every five deaths of children under age five occur in these regions.
- Children in sub-Saharan Africa are more than 15 times more likely to die before the age of 5 than children in high income countries.
- Malnourished children, particularly those with severe acute malnutrition, have a higher risk of death from common childhood illness such as diarrhoea, pneumonia, and malaria. Nutrition-related factors contribute to about 45per cent of deaths in children under-5 years of age.
Maternal health
- Over 40 per cent of all countries have fewer than 10 medical doctors per 10,000 people; over 55 per cent of countries have fewer than 40 nursing and midwifery personnel per 10,000 people.
- Every day in 2017, approximately 810 women died from preventable causes related to pregnancy and childbirth.
- 94per cent of all maternal deaths occur in low and lower middle-income countries.
- Young adolescents (ages 10-14) face a higher risk of complications and death as a result of pregnancy than other women.
HIV/AIDS, malaria and other diseases
- 38 million people globally were living with HIV in 2019.
- 25.4 million people were accessing antiretroviral therapy in 2019.
- 1.7 million people became newly infected with HIV in 2019.
- 690 000 people died from AIDS-related illnesses in 2019.
- 75.7 million people have become infected with HIV since the start of the epidemic.
- 32.7 million people have died from AIDS-related illnesses since the start of the epidemic.
- Tuberculosis remains the leading cause of death among people living with HIV, accounting for around one in three AIDS-related deaths.
- Globally, adolescent girls and young women face gender-based inequalities, exclusion, discrimination and violence, which put them at increased risk of acquiring HIV.
- HIV is the leading cause of death for women of reproductive age worldwide.
- AIDS is now the leading cause of death among adolescents (aged 10–19) in Africa and the second most common cause of death among adolescents globally.
- Over 6.2 million malaria deaths have been averted between 2000 and 2015, primarily of children under five years of age in sub-Saharan Africa. The global malaria incidence rate has fallen by an estimated 37 per cent and the mortality rates by 58 per cent.
3.1 By 2030, reduce the global maternal mortality ratio to less than 70 per 100,000 live births.
3.2 By 2030, end preventable deaths of newborns and children under 5 years of age, with all countries aiming to reduce neonatal mortality to at least as low as 12 per 1,000 live births and under-5 mortality to at least as low as 25 per 1,000 live births.
3.3 By 2030, end the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases.
3.4 By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being.
3.5 Strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol.
3.6 By 2020, halve the number of global deaths and injuries from road traffic accidents.
3.7 By 2030, ensure universal access to sexual and reproductive health-care services, including for family planning, information and education, and the integration of reproductive health into national strategies and programmes.
3.8 Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.
3.9 By 2030, substantially reduce the number of deaths and illnesses from hazardous chemicals and air, water and soil pollution and contamination.
3.A Strengthen the implementation of the World Health Organization Framework Convention on Tobacco Control in all countries, as appropriate.
3.B Support the research and development of vaccines and medicines for the communicable and noncommunicable diseases that primarily affect developing countries, provide access to affordable essential medicines and vaccines, in accordance with the Doha Declaration on the TRIPS Agreement and Public Health, which affirms the right of developing countries to use to the full the provisions in the Agreement on Trade Related Aspects of Intellectual Property Rights regarding flexibilities to protect public health, and, in particular, provide access to medicines for all.
3.C Substantially increase health financing and the recruitment, development, training and retention of the health workforce in developing countries, especially in least developed countries and small island developing States.
3.D Strengthen the capacity of all countries, in particular developing countries, for early warning, risk reduction and management of national and global health risks.
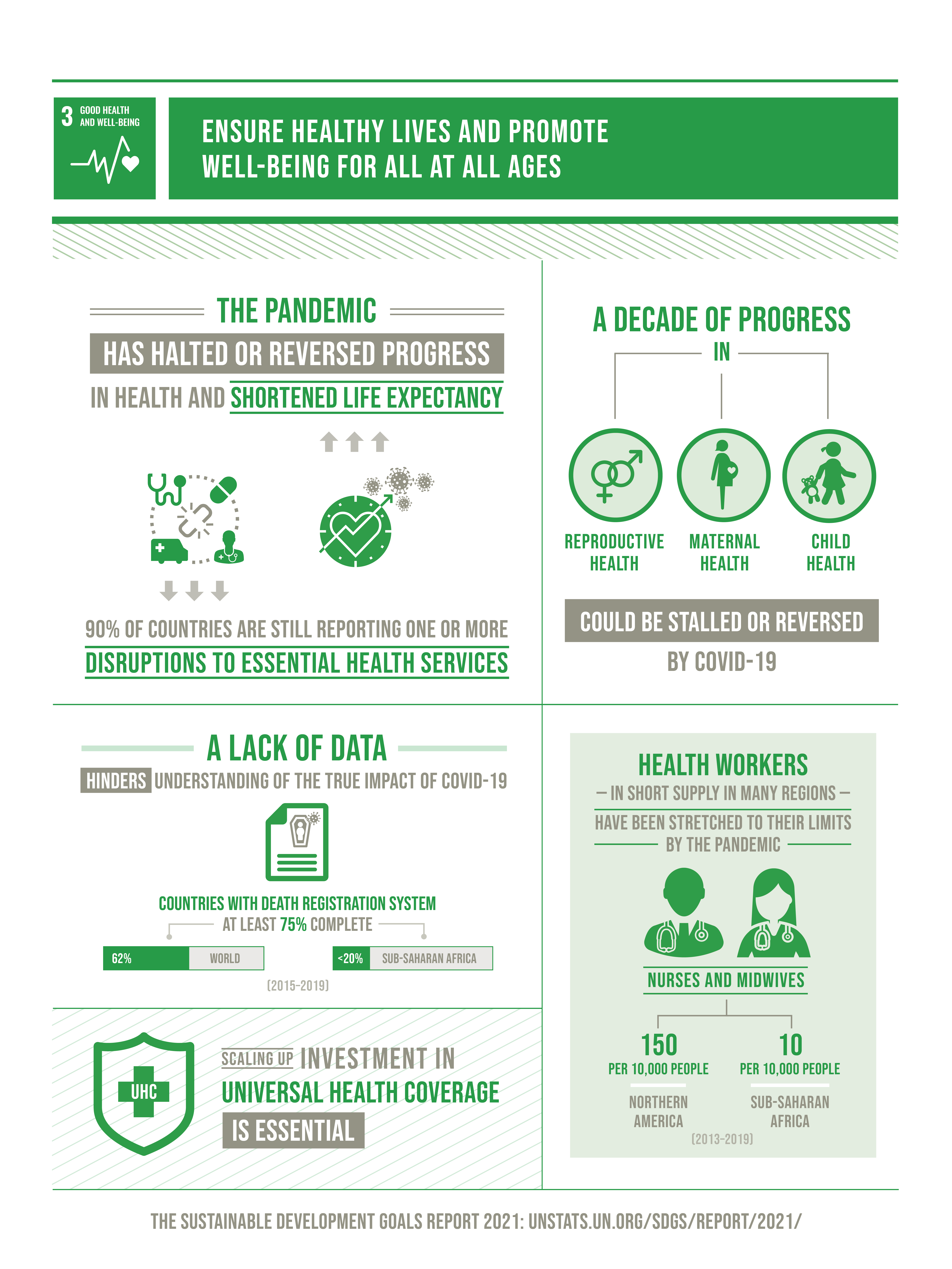
Before the COVID-19 pandemic, progress had been made in many health areas, including improving the health of mothers and children, increasing immunization coverage and reducing the incidence of communicable diseases, albeit not fast enough to meet the Goal 3 targets by 2030. The disruption caused by the pandemic has now halted progress and even reversed some gains made. According to a recent survey, substantial disruptions persist more than a year into the pandemic, with about 90 per cent of countries and territories still reporting one or more disruptions to essential health services. Among the health services most extensively affected are those for mental, neurological and substance use disorders; neglected tropical diseases; tuberculosis; HIV and hepatitis B and C; cancer screening; services for other non-communicable diseases, including hypertension and diabetes; family planning and contraception; urgent dental care; malnutrition; immunization; and malaria.
According to data from the period 2014–2020, 83 per cent of births worldwide were assisted by skilled health professionals, including medical doctors, nurses and midwives, an increase from 71 per cent in the period from 2007 to 2013. The COVID-19 pandemic may reverse gains in skilled childbirth care coverage and disrupt maternity health services.
The world has made substantial progress towards the goal of ending preventable child deaths, with the global under-5 mortality rate decreasing from 76 to 38 deaths per 1,000 live births between 2000 and 2019. The global neonatal mortality rate fell from 30 deaths to 17 per 1,000 live births in the same period. Even with such progress, 5.2 million children died in 2019 before reaching their fifth birthday, with almost half of those deaths, 2.4 million, occurring in the first month of life. While the full impact of the pandemic on child survival is not yet known, significant disruption to the continued provision of life-saving interventions could stall or even reverse the progress made.
The proportion of women of reproductive age (15 to 49 years) who have their family planning needs met by modern contraceptive methods has remained steady at around 77 per cent between 2015 and 2021, reaching only 56 per cent in sub -Saharan Africa and 52 per cent in Oceania, excluding Australia and New Zealand. The ongoing pandemic may lead to reductions in these figures as a result of supply-chain disruptions and decreased access to family planning services, while the fertility intentions and family planning needs among women of reproductive age may also change.
The global adolescent birth rate has fallen from 56 births per 1,000 adolescent women 15 to 19 years of age in 2000 to 45 births per 1,000 adolescents in 2015 and 41 per 1,000 in 2020. The declines varied considerably across regions, with the largest decrease in Central and Southern Asia from 70 births per 1,000 adolescents in 2000 to 24 births per 1,000 in 2020.
While the rate of new HIV infections declined from 0.48 infections pe r 1,000 uninfected population among adults (15 to 49 years of age) to 0.37 per 1,000 between 2010 and 2019, it remained far higher than the global target for 2020. The largest decrease was in sub-Saharan Africa, the region with the highest numbers of people living with HIV. Major inequalities remain in access to HIV prevention, testing and treatment services across regions, countries, and sub-populations within countries. There is evidence to suggest that the COVID-19 pandemic has caused considerable disruption to HIV services, including testing, initiation of treatment, voluntary medical male circumcision and pre-exposure prophylaxis.
In 2019, an estimated 10 million people fell ill with tuberculosis, of whom 56 per cent were adult men, 32 per cent adult women, 12 per cent children and 8.2 per cent people living with HIV, making it the leading cause of death from a single infectious agent. Globally, the incidence of tuberculosis fell from 174 new and relapse cases per 100,000 population in 2000 to 130 cases per 100,000 in 2019, a 25 per cent decline over the period, with the tuberculosis mortality rate among HIV-negative people falling by 45 per cent in the same period. Although the disease burden is decreasing, large gaps in detection and treatment persist, and the current pace of progress is not fast enough to meet the target of ending tuberculosis by 2030. Drug - resistant tuberculosis is a continuing threat: in 2019, there were 465,000 new cases with resistance to rifampicin, the most effective first-line drug, and 78 per cent of those infected with tuberculosis had a multidrug-resistant strain. As a result of the COVID-19 pandemic, an estimated 1.4 million fewer people received necessary care for tuberculosis during 2020 compared with the previous year, a reduction in treatment levels of 21 per cent.
Between 2015 and 2019, the incidence of malaria plateaued at around 57 cases per 1,000 people at risk. The target of the World Health Organization for reductions in malaria case incidence in 2020 will be missed by 37 per cent. In 2019, there were a total of 229 million malaria cases worldwide, with the disease claiming some 409,000 lives. Gaps in funding and in access to life-saving tools are undermining global efforts to curb the disease, and the COVID-19 pandemic is expected to set the fight back even further.
The use of the hepatitis B vaccine in infants has reduced the incidence of new chronic hepatitis B infections considerably. The proportion of children under 5 years of age who became chronically infected fell from 4.7 per cent in the pre-vaccination era to 0.9 per cent in 2020. Worldwide, the 2020 target of 1 per cent seroprevalence in children under 5 years of age has been met. Additional efforts for increasing coverage are needed to achieve the Goal target of 0.1 per cent seroprevalence by 2030.
In 2019, 1.74 billion people were reported to have required mass or individual treatment and care for neglected tropical diseases, down from 2.19 billion in 2010 and 12 million fewer than the figure reported for 2018. The lower number of people requiring interventions is largely the result of having eliminated at least one neglected tropical disease in 42 countries and territories since 2010.
Globally, 74 per cent of all deaths in 2019 were caused by non-communicable diseases. The probability of dying from any of the four main non-communicable diseases (cardiovascular disease, cancer, diabetes or chronic respiratory disease) between 30 and 70 years of age decreased from 19.9 per cent in 2010 to 17.8 per cent in 2019. The rate of decline is insufficient to meet the Goal target. The COVID-19 pandemic has underscored the need for further attention to interventions in non-communicable diseases, as people with underlying non-communicable diseases are at higher risk of severe illness and death from the COVID-19 virus.
About 700,000 suicide deaths occurred in 2019. The global suicide death rate declined by 29 per cent, from 13 deaths per 100,000 population in 2000 to 9.2 deaths per 100,000 in 2019.
In 2019, global alcohol consumption was 5.8 litres of pure alcohol per person 15 years of age or older, a 5 per cent decrease from 6.1 litres in 2010.
The global rate of mortality from road traffic injuries fell by 8.3 per cent, from 18.1 deaths per 100,000 population in 2010 to 16.7 deaths per 100,000 in 2019. Nevertheless, 1.3 million people worldwide died in road traffic accidents in 2019, 75 per cent of whom were boys and men. Low-income countries and territories had lower rates of vehicle ownership than in high-income countries and territories, yet a death rate more than 3.5 times higher. Road traffic injuries were the leading cause of death among young people 15 to 29 years of age worldwide.
The global prevalence of tobacco uses among men declined from 50 per cent in 2000 to 38.6 per cent in 2018, and among women from 16.7 per cent in 2000 to 8.5 per cent in 2018. Even so, the number of people dying from a tobacco-related illness was estimated to be more than 8.1 million in 2017.
Unintentional poisonings were responsible for more than 84,000 deaths in 2019. Although the number of such deaths has steadily declined since 2000, mortality rates continue to be relatively high in low-income countries and territories, where they are more than twice the global average. One third of all deaths from unintentional poisonings occurred in sub-Saharan Africa.
Immunization is one of the world’s most successful and cost-effective health interventions. While vaccination coverage among infants increased from 72 per cent in 2000 to 85 per cent in 2015 before stalling until 2019, an estimated 19.7 million children did not receive essential vaccines during the first year of their life in 2019. In addition, global coverage levels for the pneumococcal conjugate vaccine, which has the potential to significantly reduce the incidence of pneumonia, have yet to reach 50 per cent. Measles is a highly contagious disease, and the 71 per cent coverage of the two-dose vaccine in 2019 was insufficient to prevent outbreaks of measles.
Improvements in essential health services, as measured by the universal health coverage service coverage index, increased from a global average of 45 out of 100 in the year 2000 to 66 in 2017. Low-income countries and territories experienced the greatest progress, driven mainly by interventions for infectious diseases. However, the pace of progress has slowed since 2010, and the poorest countries and territories and those affected by conflict are generally lagging furthest behind. The COVID-19 pandemic is derailing progress even further.
Before the pandemic, an estimated 927 million people, or 12.7 per cent of the global population, made out-of-pocket health-care payments amounting to more than 10 per cent of their household budgets, and for 209 million people, or 3 per cent, their share of health-care spending exceeded 25 per cent of their household budgets, posing an even greater threat to spending on other essential goods and services such as food and education.
ODA for basic health from all official donors has increased by 59 per cent in real terms since 2010, reaching $11 billion in 2019. The Global Fund to Fight AIDS, Tuberculosis and Malaria, the Gavi Alliance and the United States of America accounted for more than half of that total, providing $2.4 billion, $1.9 billion and $1.8 billion, respectively. In 2019, $3.4 billion was spent on basic health care, $2.2 billion on infectious disease control, excluding HIV/AIDS, and $2.2 billion on malaria control.
Health workers are on the front line of the COVID-19 pandemic response. Countries and territories, especially those with a limited health workforce, are further constrained with regard to the delivery of essential health services. On the basis of data from the period 2013–2018, the density of nursing and midwifery personnel in Northern America is more than 150 per 10,000 population, which is more than 15 times that in sub-Saharan African and 8 times that in Northern Africa and Southern Asia. The density of medical doctors in Northern America, Oceania and Central Asia remains around 25 per 10,000 population, compared to 2 per 10,000 population in sub-Saharan African.
Ensuring healthy lives for all requires a strong commitment, but the benefits outweigh the cost. Healthy people are the foundation for healthy economies. Immunization is one of the world’s most successful and cost-effective health interventions. While vaccination coverage among infants increased from 72 per cent in 2000 to 86 per cent in 2018, an estimated 19.4 million children did not receive the essential vaccines during the first year of life. In fact, since March 2020, routine childhood immunization services have been disrupted on a scale not seen since the inception of the Expanded Programme on Immunization in the 1970s.
You can start by promoting and protecting your own health and the health of those around you, by making well-informed choices, practicing safe sex and vaccinating your children. You can raise awareness in your community about the importance of good health, healthy lifestyles as well as people’s right to quality health care services, especially for the most vulnerable such as women and children. You can also hold your government, local leaders and other decisionmakers accountable to their commitments to improve people’s access to health and health care.
[Source:- www.un.org]